Most of us have a general awareness of cholesterol as a marker of health. But what do cholesterol values truly mean, and when do we need extra help managing them in the form of cholesterol medication?
Today we’ll take a deep-dive into how we evaluate cholesterol, what “high cholesterol” means, and at what cholesterol level medication is required.
Why Cholesterol Is Tricky
First things first: cholesterol has a bad reputation in most people’s minds.
The truth is, cholesterol is both made in our liver and a vital nutrient that helps us produce hormones, the walls of our cells, and Vitamin D, to name a few. Therefore, we’re never hoping to eliminate cholesterol entirely.
While it’s essential to take an appropriate amount of cholesterol medication if, indeed, you need it, we have to be cautious not to lower cholesterol too much. If we do, the treatment can actually inhibit other bodily processes that are extremely important for your well-being.
To determine at what level cholesterol medication is required, we have guidelines based on the general population and on a subset of the general population — people with heart disease.
These guidelines can be tricky, because talking about cholesterol without individualizing the numbers is a bit like forcing everyone to shop in a department store full of “one-size-fits-all” clothing. Sure, a few people will find items that fit them perfectly. The vast majority, however, will end up with ill-fitting garments that don’t quite do the job.
“High Cholesterol,” Defined
We can view some things in life simply by looking at a bottom-line number. Cholesterol isn’t one of those things.
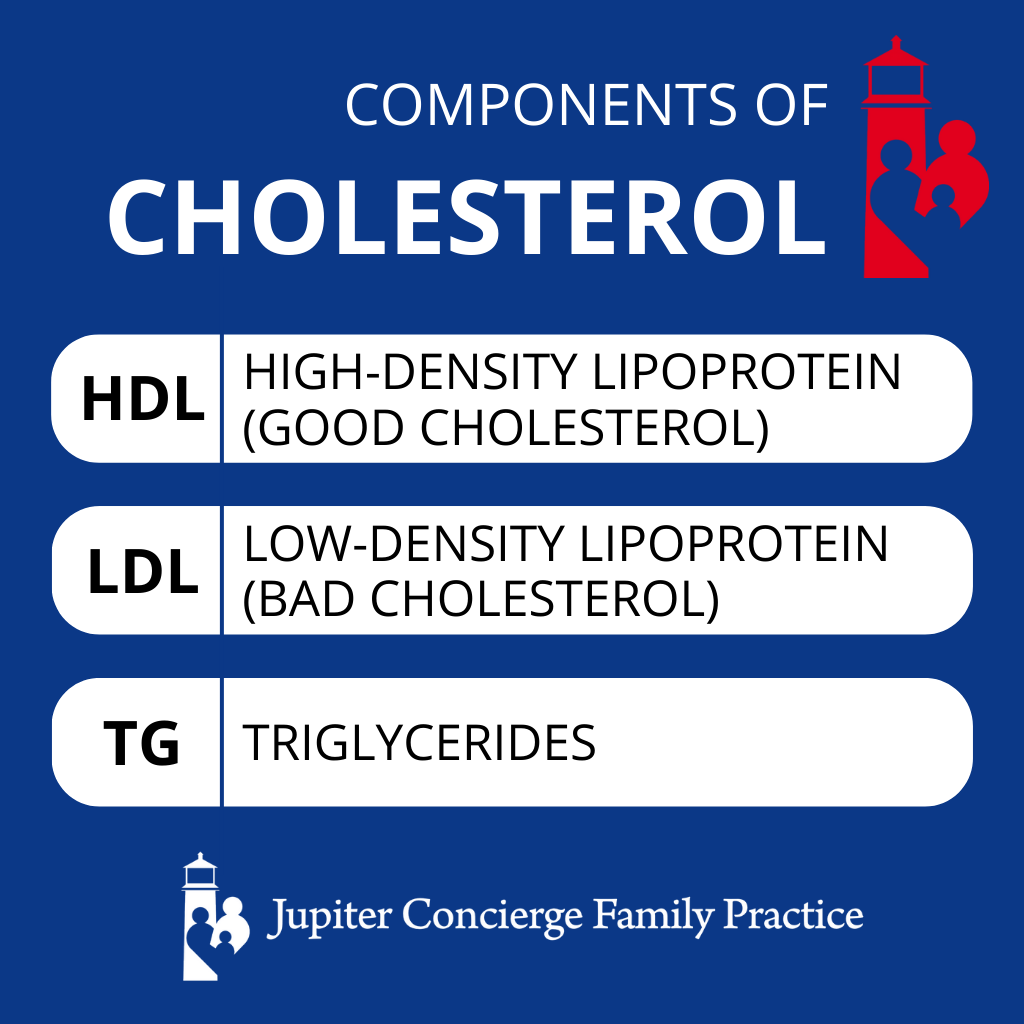
The technical definition of high cholesterol is a total reading of 200 or greater. The problem with that definition is that total cholesterol doesn’t tell the whole story. Total cholesterol actually measures three crucial components:
- HDL — high-density lipoprotein, also known as “good cholesterol”
- LDL — low-density lipoprotein, also known as “bad cholesterol”
- TG — triglycerides, what excess fat is stored as, also “bad cholesterol”
LDL is considered “bad” because it forms the plaque that can block arteries. TG gives your body energy, but high TG levels can cause hardening (or sclerosing) of blood vessels and lead to cardiovascular problems like heart attack or stroke.
High HDL, however, is wonderful and even protective for your health, helping your liver process and get rid of excess LDL cholesterol.
When we look beyond total cholesterol, we can consider the goal values for each individual component:
- HDL — Above 40 in men and above 50 in women. Anything over 60 is excellent and protective.
- LDL — Less than 160 if you don’t have a cardiac risk, and less than 100 if you do have cardiac risk. If you have known heart disease, we want to see LDL less than 70, or perhaps even 50 according to some new research.
- TG — Below 150, but preferably below 100.
This is why I don’t simply look at total cholesterol. Total cholesterol may appear abnormal (over 200), but the individual components may be just fine. Perhaps a patient has an HDL of 150. That may cause the total number to exceed the recommended maximum, but there’s actually nothing wrong with very high HDL.
As far as total cholesterol, one concern when I’m evaluating my patients’ cholesterol panels is that the total doesn’t get below 150. Remember, when cholesterol levels get too low, hormone pathways and function become disrupted. When someone doesn’t have heart disease — or risk factors of heart disease — very low cholesterol can cause unnecessary problems.
That said, in the case of heart disease, we’re willing to take the risks of low cholesterol over high cholesterol. It’s more important to keep the arteries free of blockage in cardiac patients because blocked arteries are much more life-threatening.
At What Level of Cholesterol Is Medication Required?
So how do we lower high cholesterol, and at what level is medication required?
Many people’s numbers improve with the powerful interventions of diet and exercise. Healthy eating and healthy movement can radically shift our lipid profile.
In some cases, though, that’s not enough. If diet and exercise aren’t creating meaningful shifts in a patient’s cholesterol, or if the problem is too urgent to wait for lifestyle measures to take effect, it’s probably time to look at medication.
Generally speaking, an LDL over 190 warrants medication, regardless of cardiac risk. LDL in the 130–190 range is what I call “the gray zone.” It’s best keeping an eye on and implementing dietary and exercise measures if you haven’t already.
When a person has heart disease — meaning there’s proof of blocked arteries — the target LDL should be lower than 70, perhaps even lower than 50 based on some recent studies.
It’s possible to achieve this with diet and exercise, but many times, it requires a medication known as a statin.
Statins, or HMG-CoA reductase inhibitors, come in different strengths of ability to lower LDL. They also have side effects; for example, many of them can cause muscle pains. However, statins are very effective at helping prevent the production of cholesterol.
When a cholesterol-lowering medicine is necessary, but side effects make a statin untenable, another option is a class of medication that works on genes. These are PSCK9 inhibitors, such as Repatha and Praluent. They work by increasing the clearance of LDL cholesterol, which is another way of saying they allow LDL to be packaged and disposed of.
Both drugs can help lower LDL cholesterol, one by preventing its production and the other by promoting its elimination.
How Important Is Cholesterol in Heart Disease?
Ultimately, what we really want to know about cholesterol is how it affects our health. How much should you worry about high LDL with regard to heart attack and stroke? How safe should you feel if you have low LDL?
In reality, there are many, many important risk factors other than cholesterol that contribute to heart disease. Cholesterol is a factor, yes, but perhaps only 30% of the risk, which means another 70% is not cholesterol.
Things like metabolic and genetic predispositions, C-reactive protein, inflammation levels, smoking/vaping status, oxidative stress levels, and quality of foods — just to name a few — have a significant bearing on heart disease.
So, yes, cholesterol levels and ratios are important markers for cardiac health, but they’re not the only markers. And remember: Cholesterol itself is physiologically vital. We need it in order to be healthy. We simply need it in the right amounts and ratios.


Dr. David Rosenberg
Dr. Rosenberg is a board-certified Family Physician. He received his medical degree from the University of Miami in 1988 and completed his residency in Family Medicine at The Washington Hospital in Washington, Pennsylvania in 1991. After practicing Emergency Medicine at Palm Beach Gardens Medical Center for two years, he started private practice in Jupiter, in 1993. He is an avid baseball fan and Beatles fanatic, since he was 8 years old. He has been married to his wife, Mary, since 1985 and has three grown children.
David completed additional studies at Mercer University, Macon, Georgia and obtained a BS in Chemistry in 1983.
“My interests include tennis, snow skiing, Pilates and self-development.”

Subscribe to our Newsletter!
Receive latest blog posts, health tips, and exclusive offers from Jupiter Concierge Family Practice straight to your inbox.