There’s a reason you’ve likely heard about “long-haul COVID.”
Various studies show that, regardless of symptom severity, 20–30% of COVID patients get what’s known as “long-haul COVID.”
But what is long-haul COVID — what are its defining characteristics and lasting symptoms? And if you develop it, what options are there for long-haul COVID treatment?
What Is “Long-Haul” COVID?
As the name implies, long-haul COVID occurs when certain COVID symptoms just don’t go away. In long-haul COVID, the initial COVID illness is over — the fever is gone, the virus is out of your system, and the acute aspects of the upper respiratory infection we call “COVID” have resolved.
But with long-haul COVID (sometimes just called “long COVID” or post-COVID syndrome), certain symptoms last for longer than a month. They can persist for several months before resolving, possibly years. Of course, since COVID is relatively new, we’re still not certain how it looks over an extended period of time.
The issue with COVID is that it can stimulate the immune system to the point of overreaction, resulting in a cascade of immune responses that cause damage to the body’s systems. So instead of helping you recover, your immune system actually harms you.
Even when the virus itself is long gone, the continuing immune response keeps causing problems. That’s long-haul COVID in a nutshell.
Long-Haul COVID Symptoms
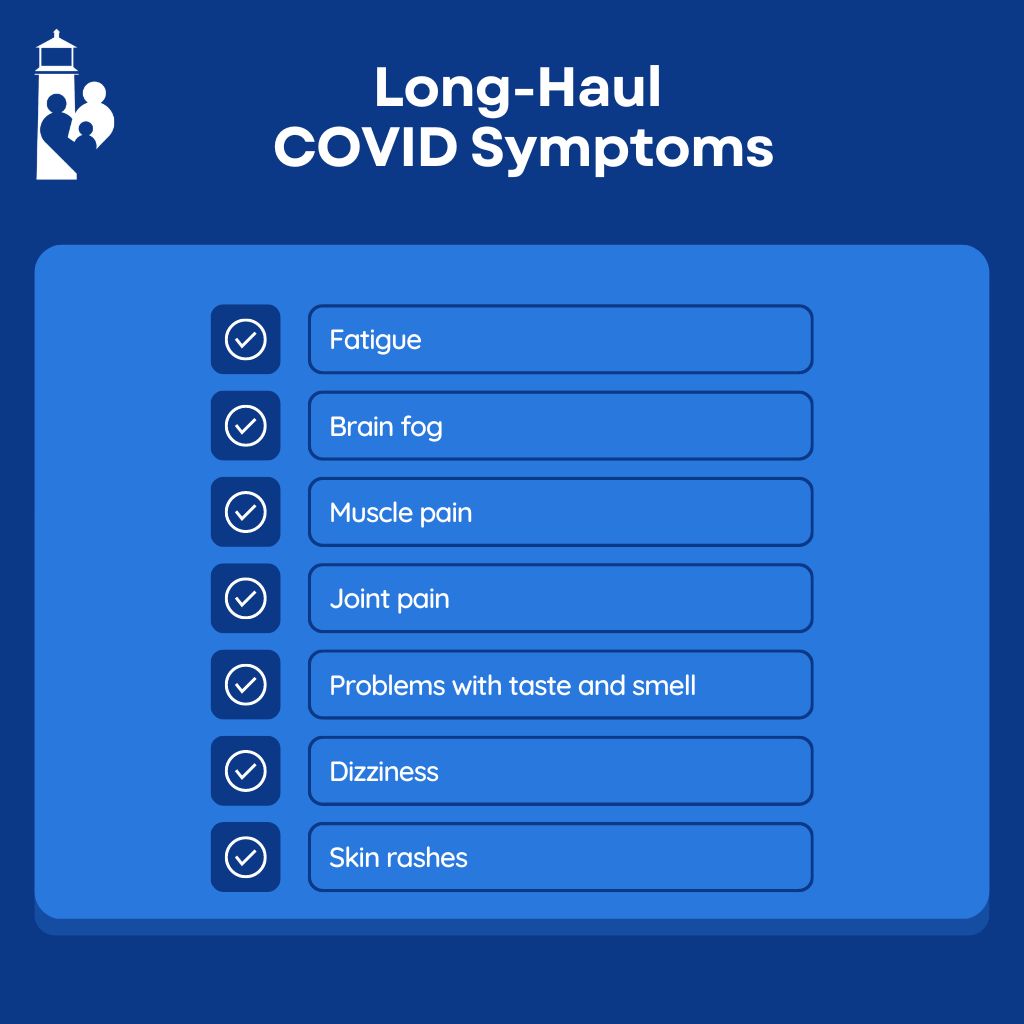
Long-haul COVID symptoms differ somewhat from the acute symptoms of infection. You may experience a fairly wide range of symptoms, including:
- Fatigue
- Brain fog
- Muscle pain
- Joint pain
- Problems with taste and smell
- Dizziness
- Skin rashes
You may have some or all of these symptoms, or you may experience others. We’re still learning about long-haul COVID and documenting additional symptoms, such as sleep disturbances.
Long-Haul COVID Treatment
If you find yourself facing long-haul COVID after your acute infection has subsided, there are things you can do to help your body recuperate.
Because long-haul COVID is an immune response gone awry, treatments aim to support the immune system so that it causes less damage to the body. Below are some examples of tangible steps you can take to support your reeling immune system.
Food as Medicine
Certain nutrients are very helpful in combating long-haul COVID because they help feed your body’s repair system. These include:
- Vitamin D3
- Curcumin
- NAC
- Lipoic acid
- Resveratrol
- B-complex
- Green tea extract
Another sound food move when addressing long-haul COVID is to ensure your diet doesn’t promote inflammation. Avoid pro-inflammatories like dairy, gluten, and sugar. If that has you scratching your head, consider consulting a dietitian to help you find alternatives that work for you.
Lifestyle Choices
The persistent immune response characteristic of long-haul COVID kicks off other disease processes as well, such as an imbalance of the microbiome (good and bad bacteria) in your gut or inflammation in different parts of the body. The way you live your life can exacerbate these secondary problems, or help mitigate them.
For example, now is not the time to engage in strenuous physical activity, like training for a marathon. Trying to “push through” long COVID isn’t going to work. Overexercise causes excess inflammation — something a person with long-haul COVID is both actively trying to reduce and is less equipped to recover from than usual.
If you have long-haul COVID, you aren’t your usual self. Adjusting your lifestyle choices so that they aren’t hindering your recovery is important.
Prevention Is Still the Best Medicine
COVID is becoming more widespread — and compared to its beginnings in 2019, it’s also less deadly. As the mortality and hospitalization rates decline, people can begin to feel like it’s no longer something they need to avoid.
While it’s a relief that COVID isn’t currently as life-threatening as it was, it can still have long-term consequences. Post-COVID syndrome is surprisingly common, and while we have a few helpful treatments for long-haul COVID, we don’t have a guaranteed cure. Your best option is still taking precautions and avoiding COVID altogether.
If you do get COVID, do your part to prevent transmission. Take a test when you have symptoms, stay home, and avoid gatherings until you’re no longer contagious.

Dr. David Rosenberg
Dr. Rosenberg is a board-certified Family Physician who obtained a BS in Chemistry at Georgia's Mercer University in 1983 and a medical degree from the University of Miami in 1988. He completed his residency in Family Medicine at The Washington Hospital in Washington, Pennsylvania, in 1991 and then practiced Emergency Medicine at Palm Beach Gardens Medical Center for two years. In 1993 he started private practice in Jupiter.
Dr. Rosenberg has been married to his wife Mary for 38 years and they have three grown children together. Some of his interests include being a huge baseball fan, sailing, snow skiing, self-development, and learning to play piano.